Open enrollment for the New Jersey health insurance marketplace, GetCoveredNJ, officially began on November 1st for the 2022 coverage year.[i] With expanded financial aid through state subsidies and the Affordable Care Act’s Medicaid Expansion, health insurance affordability continues to improve for the Garden State’s low- and middle-income residents.[ii] Yet, for many, challenges to getting and maintaining coverage persist. On top of pre-pandemic disparities in health coverage and the unequal impact of the pandemic, the looming end of federal public health emergency (PHE) assistance could exacerbate health coverage disparities.[iii]
This report looks at data from the past year to examine trends in who remains uninsured and who would benefit or be harmed by changes in public health insurance policies. The findings show that health coverage rates differ across racial, age, income, education, and geographic lines. Structural inequalities — such as limited access to affordable coverage through jobs, difficulties saving due to low wages, and transportation challenges — reduce access to coverage options and perpetuate health insurance inequities. The report ends with recommendations to bridge coverage barriers through improved outreach, communication, and affordability.
Hispanic/Latinx and Black Residents Continue to Face Barriers to Coverage
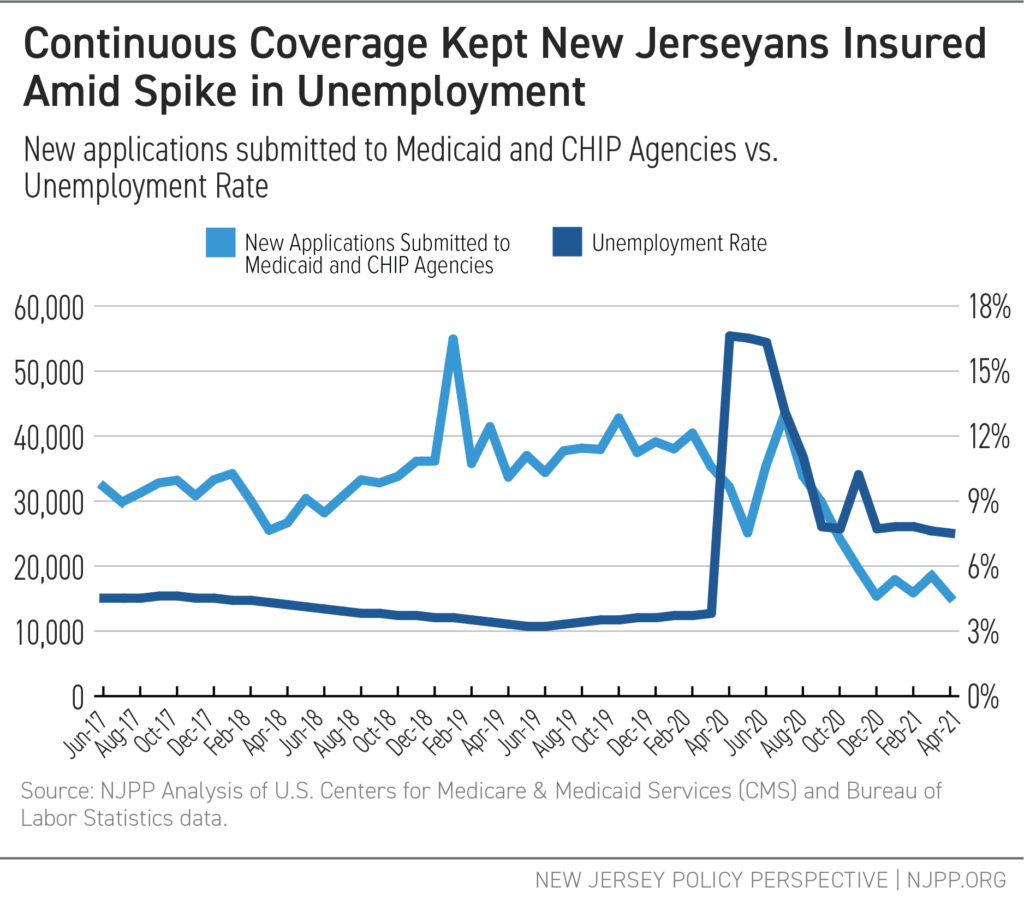
Since the introduction of the Affordable Care Act (ACA), uninsured rates for families of color have improved significantly.[iv] Even during the COVID-19 pandemic, federal and state efforts have helped get and keep people enrolled in health care coverage through policies like continuous coverage in Medicaid and increased premium subsidies for Marketplace plans.[v] However, as federal relief policies end, the increased risk of coverage loss disproportionately harms Hispanic/Latinx and Black residents, many of whom were already at greater risk of being uninsured before the pandemic.
In New Jersey, Hispanic/Latinx and Black residents remain most vulnerable to changes in federal and state coverage policy due to eligibility restrictions and disparities in access to employer-based insurance. Rooted in a history of systemic racism and structural inequalities in access to coverage, families of color face disproportionate barriers to health care. For instance, Hispanic/Latinx and Black residents are more likely to be employed in part-time jobs that lack benefits and affordable coverage or have their hours cut below benefit thresholds.[vi] Additionally, Black residents are most likely to get their coverage through public programs because of limitations on access to employer-based coverage.
Undocumented immigrants have also been left behind throughout the pandemic, as they remain ineligible for Medicaid or Marketplace coverage — the very programs that have helped so many families keep their coverage.
Residents with Limited Access to Employer-Based Coverage are More Likely to Lack Health Insurance Coverage
Employers who pay low wages rarely provide robust health insurance benefits. For instance, just 24 percent of U.S. workers in the lowest wage jobs had access to medical benefits through their employer in 2019.[vii] Consequently, if low-paid workers don’t qualify for Medicaid, they must make tough choices about costly health insurance options.
If a worker’s employer-based plan remains within the ACA’s affordability threshold (9.83 percent of household income for 2021), additional family coverage often costs significantly more.[viii] This is due to what is called a “family glitch,” when a workers’ individual insurance option qualifies as “affordable,” and, as a result, their family members are not eligible for subsidies on the Marketplace. Currently, around 55,000 New Jerseyans are stuck in this “family glitch,” with no access to affordable family coverage.[ix]
Structural inequities exist not only in access to employer-based coverage but also with public coverage options. Due to less flexible or unpredictable work hours, limited access to transportation, and fewer resources for information, those most in need of public coverage also have the most obstacles to obtain that coverage.[x]
For low-income residents making less than $25,000 per year, the harms caused by these obstacles to coverage are stark. Low-income residents are three times more likely to be uninsured than someone making between $50,000 and $74,999, and six times more likely than someone making between $100,000 and $149,999.
Additionally, residents with less than a high school diploma are eight times more likely to be uninsured than someone with at least a Bachelor’s degree. The same patterns follow for public health coverage: residents with less than a high school diploma are twice as likely to be enrolled in public coverage than those with a Bachelor’s degree or higher. In contrast, those making less than $25,000 are three times more likely to be enrolled in public coverage than those who make between $100,000 and $149,999.
Young Adults Remain Most Uninsured Age Group, Despite Pandemic Efforts
In addition to income and education playing an outsized role in health insurance coverage, age is also a determining factor. Young adults in New Jersey are more likely to be uninsured and less likely than other age groups to participate in a public insurance program. There are several reasons why young people are more likely to struggle to get covered: lack of access to employer-based coverage, less stable employment as they first enter the workforce, a lack of knowledge about affordable options after losing coverage through their parents’ insurance at 26, and fewer savings and a greater need for help from family with regular bills.[xi]
Coverage Rates Vary Widely Across Counties
While Household Pulse Survey data from this past year only provides state-level estimates, pre-pandemic coverage rates showed significant differences in coverage across counties. Counties that have more families with lower incomes, limited access to employer coverage, or restrictions on coverage due to immigration status were more likely to see higher numbers of uninsured residents, especially for their working-age adults. Uninsured rates for this group range from a low of 3.6 percent in Sussex County to a high of 19.8 percent in Passaic County.
Recommendations: Outreach and Enrollment Efforts Should Boost Health Coverage
Barriers to health coverage keep thousands of New Jerseyans uninsured, leaving residents unable to access or afford needed care. To address coverage gaps and get people access to the care they need, state leaders should take several proactive steps:
Plan Diverse Communications and Outreach Initiatives
As state officials and Navigator organizations begin to help participants research and understand their coverage options, they should plan to actively address existing disparities in coverage. Taking into account who is uninsured and the specific channels of communication they may turn to for information — such as community, family, medical leaders, social media, or information sessions with bilingual options — will help connect New Jerseyans with coverage in a way that meets their needs.
Simplify Enrollment Processes
Many New Jerseyans who are eligible for public insurance programs, like Medicaid and the Children’s Health Insurance Program (CHIP), face obstacles to enrollment through onerous documentation requirements, difficulty reaching a live person for questions about the process, and language barriers. The time required to overcome these challenges, particularly when many families may be applying to other programs such as Temporary Assistance for Needy Families (TANF) or the Supplemental Nutrition Assistance Program (SNAP), prohibits many New Jerseyans from enrolling, even when they are eligible. Creating an Easy Enrollment system can help to connect more New Jerseyans with affordable coverage. This system can provide residents with their health coverage options if they check a box on their tax forms, ensure automatic enrollment for those who are eligible for Medicaid, and share information about coverage options whenever a change in circumstances, like unemployment, occurs. Additionally, streamlining data-sharing across public programs can help to lessen the time required for applicants by reducing duplication of documentation efforts.
Expand Eligibility to Medicaid and CHIP
Only when all New Jerseyans are eligible for affordable health insurance will we be able to achieve universal coverage. By fully implementing the Cover All Kids initiative passed in June 2021, expanding Medicaid coverage to all residents, providing GetCoveredNJ plan options for undocumented immigrants, and restructuring the plan system to ensure that no segregation in the options or quality of care exists, state leaders can ensure that New Jersey fully embodies the value of health care as a human right.
End Notes
[i] GetCoveredNJ. Official website. https://www.nj.gov/getcoverednj/
[ii] GetCoveredNJ. “Get Financial Help.” https://nj.gov/getcoverednj/financialhelp/gethelp/
[iii] New Jersey Policy Perspective (2021). “Maintaining Continuous Medicaid Coverage After the Pandemic Would Advance Health Equity.” https://www.njpp.org/publications/blog-category/maintaining-continuous-medicaid-coverage-after-the-pandemic-would-advance-health-equity/
[iv] NJ Spotlight (2020). “Affordable Care Act Has Upped Racial Equity in NJ’s Health Care Coverage, Access.”. https://www.njspotlightnews.org/2020/01/boosting-racial-equity-in-njs-health-care-coverage-access/
[v] Ibid.
[vi] New Jersey Policy Perspective (2021). “Labor Day Snapshot: New Jersey’s Uneven Recovery.” https://www.njpp.org/publications/report/labor-day-snapshot-new-jerseys-uneven-recovery/
[vii] U.S. Bureau of Labor Statistics (2020). “Lower-wage workers less likely than other workers to have medical care benefits.” Data examines private Industry employment in 2019. https://www.bls.gov/opub/ted/2020/lower-wage-workers-less-likely-than-other-workers-to-have-medical-care-benefits-in-2019.htm
[viii] Healthinsurance.org (2021). “How Millions were Left Behind by ACA’s ‘Family Glitch’.” https://www.healthinsurance.org/obamacare/no-family-left-behind-by-obamacare/
[ix] Urban Institute (2021). “Changing the “Family Glitch” Would Make Health Coverage More Affordable for Many Families.” https://www.urban.org/sites/default/files/publication/104223/changing-the-family-glitch-would-make-health-coverage-more-affordable-for-many-families.pdf
[x] Brookings Institute (2020). “Unpredictable work hours and volatile incomes are long-term risks for American workers.” https://www.brookings.edu/blog/up-front/2020/08/18/unpredictable-work-hours-and-volatile-incomes-are-long-term-risks-for-american-workers/; Urban Institute (2020). “Access to Opportunity through Equitable Transportation.” https://www.urban.org/sites/default/files/publication/102992/access-to-opportunity-through-equitable-transportation_0.pdf; Federal Reserve Bank of Philadelphia (2018). “Accessing Economic Opportunity: Public Transit, Job Access, and Equitable Economic Development in Three Medium-Sized Regions.” https://www.philadelphiafed.org/-/media/frbp/assets/community-development/reports/accessing-economic-opportunity/1218-accessing-economic-opportunity.pdf
[xi] Urban Institute (2021). “Impacts of the ACA’s Medicaid Expansion on Health Insurance Coverage and Health Care Access among Young Adults.” https://www.urban.org/research/publication/impacts-acas-medicaid-expansion-health-insurance-coverage-and-health-care-access-among-young-adults; Pew Research Center (2019). “Majority of Americans Say Parents Are Doing Too Much for Their Young Adult Children.” https://www.pewresearch.org/social-trends/2019/10/23/majority-of-americans-say-parents-are-doing-too-much-for-their-young-adult-children/