Medicaid provides a crucial safety net for families experiencing economic hardship and saves thousands of lives during public health crises like the COVID-19 pandemic. With the federal pandemic public health emergency (PHE) extended again on October 15th, but expected to expire in early 2022, the upcoming return to pre-pandemic redetermination processes and rules on continuous enrollment threatens families’ health insurance coverage.
Thousands of New Jerseyans at Risk of Losing Health Coverage
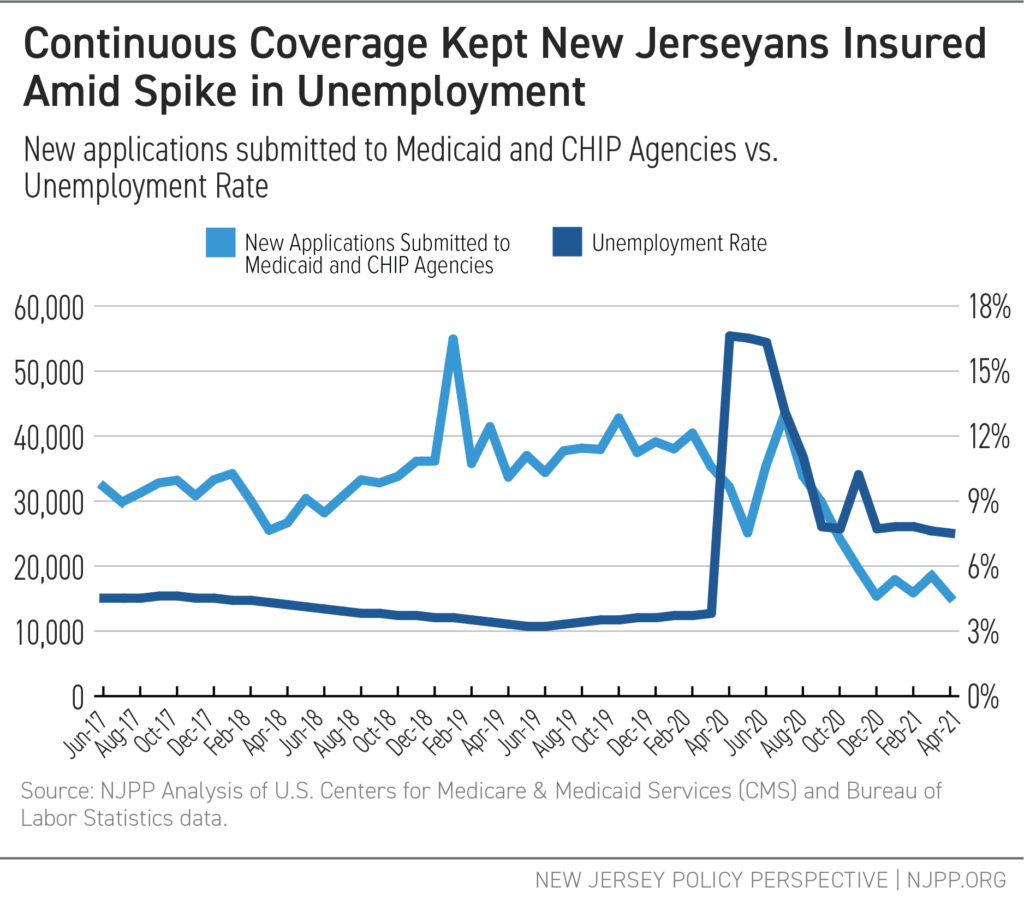
Thousands of New Jerseyans have turned to NJ FamilyCare, New Jersey’s Medicaid program, for health coverage and stability during the COVID-19 crisis. As a result, non-elderly enrollment in Medicaid grew an average of 1.9 percent per month during the first months of the pandemic. Many New Jerseyans were able to maintain continuous Medicaid coverage, regardless of changes in circumstances, thanks to federal pandemic relief policies.
New Medicaid applications have now fallen below pre-pandemic levels, a positive sign and reflection of how pandemic relief policies have protected many of those who may otherwise have exited and then re-entered Medicaid in a short period of time due to unstable employment and income.
However, around 320,000 New Jerseyans will lose Medicaid coverage in 2022 with the reintroduction of eligibility processes and the end of continuous coverage, resulting in a 19 percent decrease in enrollment compared to the end of 2021. Disenrollment from NJ FamilyCare will jeopardize health insurance for residents with low incomes. It will also disproportionately threaten the coverage of Black, Hispanic/Latinx, and mixed race families, who are disproportionately represented in the program and are more likely to experience housing and employment instability, limiting their ability to complete redetermination processes that require extensive and onerous documentation, workday commitments, or mailed notifications.
To Prioritize Equity, New Jersey Must Plan Proactively
The harms created by the sudden end of the PHE and return to normal eligibility processes necessitate state plans that center health equity. New Jersey decision makers can reduce adverse effects with several measures:
Use a 12-Month Timeline for Disenrollments
Guidance from the Centers for Medicare & Medicaid Services (CMS) allows states to take up to 12 months to return to normal income eligibility after the month in which the PHE ends, but states may choose to implement this more quickly. A slower rate for disenrollment would allow more time for beneficiaries to complete the redetermination process, fully understand their other options if they are no longer eligible, and plan for next steps in maintaining health insurance coverage.
Create and implement a communication strategy that meets people where they’re at
Complicated forms, extensive documentation requirements, and language access issues make it difficult for Medicaid beneficiaries to meet the necessary requirements of redetermination, even if they are still eligible. Actively addressing these barriers through strategies like pre-populated forms, state officials can better serve the diverse population that relies on Medicaid.
Partner with Navigator organizations and other community groups to amplify messaging and build trust
Many New Jerseyans turn to community organizations and local leaders that they trust for health insurance information. By following a structured, data-driven plan that includes clear guidance and resources for outreach to Navigators, the state can use communication channels that already exist and reach many residents who may otherwise miss the department’s messaging.
Explore Continuous Coverage, Autorenewal, and Other Coverage Opportunities
Addressing instability in Medicaid coverage requires advancing technology and policies that provide greater flexibility under changing circumstances. The state can explore a Section 1115 demonstration waiver to extend Medicaid’s 12-month continuous eligibility to adults, similar to the coverage currently provided to children. It can also improve data-sharing across state departments to simplify and efficiently process automatic renewals. Finally, clear communication or easy transfers to other insurance options for those determined to be ineligible for Medicaid — as many will be eligible for the Children’s Health Insurance Program (CHIP) or subsidized marketplace coverage through GetCoveredNJ — can help keep families covered.

