To read a PDF version of this report, click here.
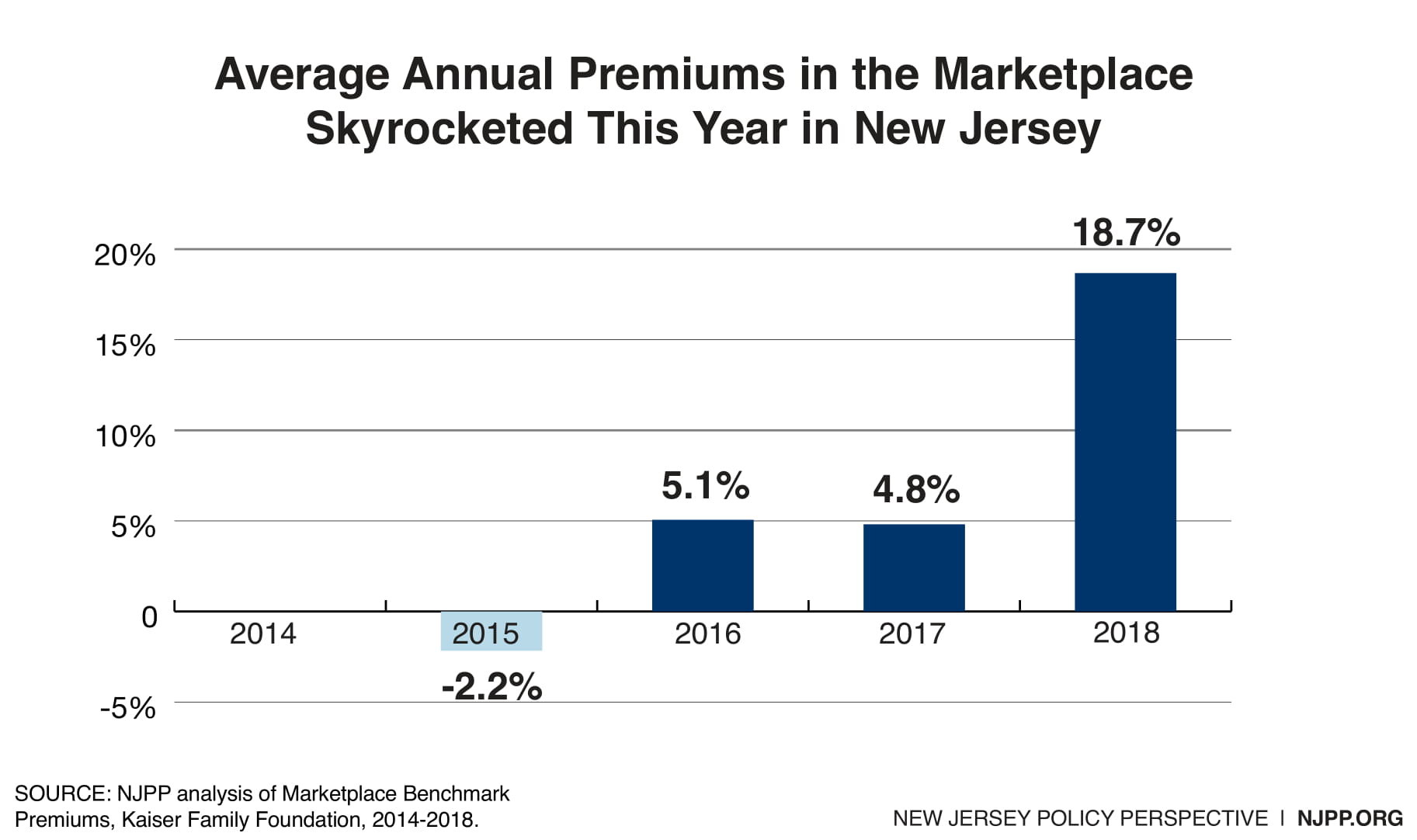
Despite recent progress made by New Jersey to keep health care coverage more affordable, the Trump administration continues to come up with new and harmful ways to do just the opposite. In New Jersey, premiums have already increased by about 20 percent in 2018 and enrollment in the individual market dropped by an unprecedented 40,000 residents. These newest actions would further undermine the health care marketplace, make insurance unaffordable for many more New Jerseyans, and could even increase the uninsured rate, which has dropped by about a third due to the Affordable Care Act (ACA).
There is a long list of actions the Trump administration has already taken to sabotage the ACA, but the most recent include the following:
1. Payments for New Jerseyans with the most serious health conditions in the individual and small employer market are halted
The Trump administration indefinitely suspended $64 million in payments to insurers in New Jersey to defray the cost of covering consumers with high health costs in 2017 in the individual and small (employer) group markets. The decision by the Centers of Medicare and Medicaid Services (CMS) not to redistribute funds to insurers for high need consumers, who often have preexisting conditions, is based on their refusal to challenge or remedy a court decision in New Mexico that invalidated their methodology for distributing “risk adjustment” payments. Those payments were to be made to insurers to compensate them for consumers who are, on average, unhealthier and therefore have higher medical costs. The federal government does not save any money for halting these payments because they are paid by other insurers that have healthier consumers.
Risk adjustment payments are necessary as the ACA requires that insurers accept anyone with pre-existing conditions. Because some insurers end up assisting more of these and other, sicker consumers than other insurers, they need additional compensation for those higher costs. These payments are crucial as they are the only remaining mechanism to compensate insurers for higher than usual consumer costs. Reinsurance ended in 2016 and Republicans in Congress defunded the risk corridor program in 2013.
While a system without risk adjustment payments creates winners and losers in the short term, all insurers lose in the long run because those insurers that have relatively healthy consumers in one year may have more unhealthy consumers in subsequent years. Because of the uncertainly of these payments, there will be pressure on all insurers to increase premiums next year. Ironically, in the CMS announcement about halting the payments, it praised the effectiveness of risk adjustment which has been in operation for three years. By suspending the payments indefinitely, CMS has caused more uncertainty in the individual and small group (employer) market which will lead to higher premiums unless this matter is resolved.
2. Federal funds for outreach slashed to near nothing
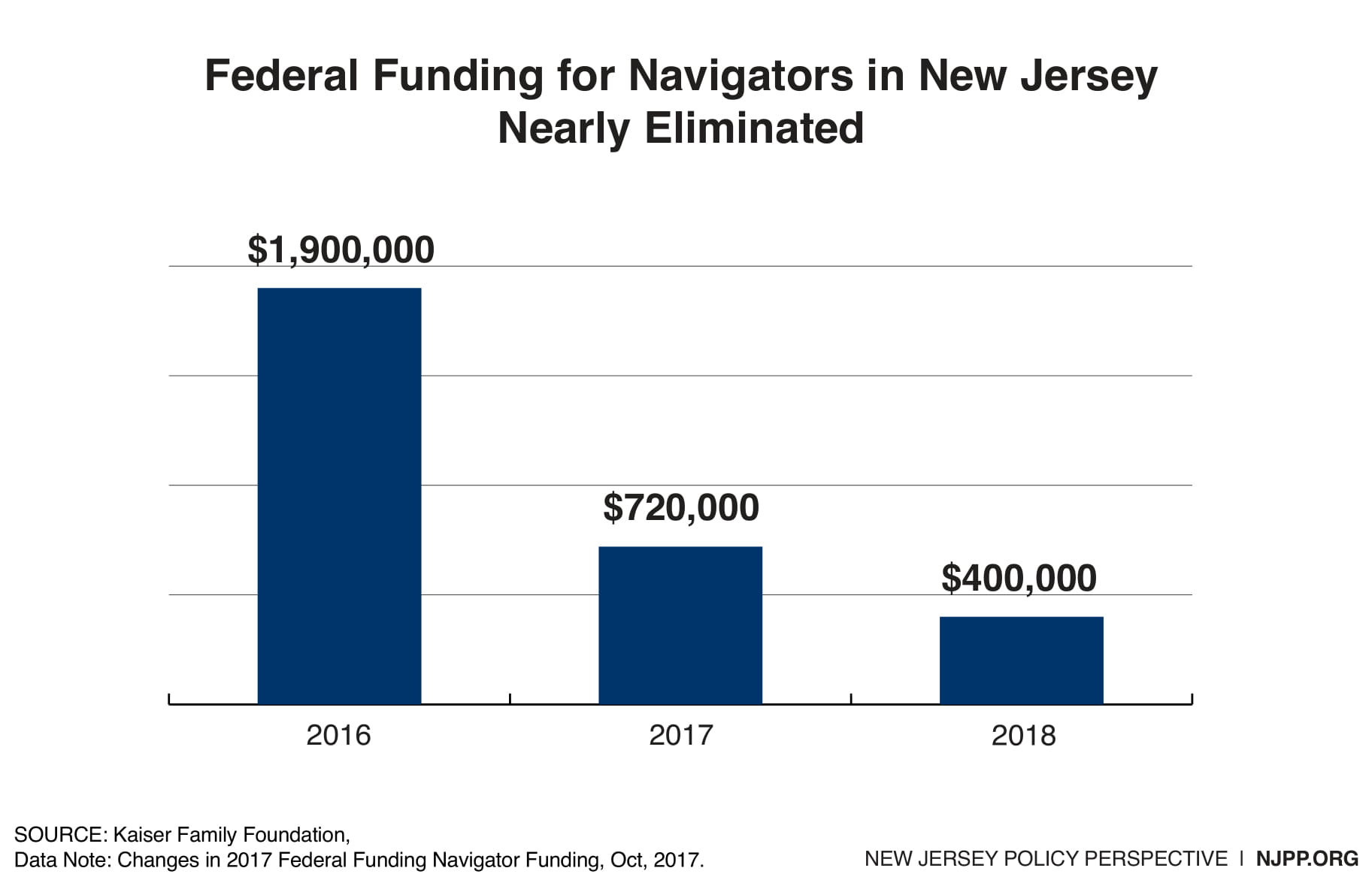
A few days after announcing the suspension of the risk adjustment payments, CMS announced that they were also slashing funding for navigators who help New Jerseyans with signing up for insurance and outreach. New Jersey’s funding was already cut 61 percent last year, decreasing the state’s allotment from $1.9 million to $720,000, one of the steepest declines in the nation. CMS’s decision to lower national funding next year by another 70 percent would result in New Jersey only receiving about $400,000. In effect, this would result in no meaningful outreach and assistance statewide.
3. Trump’s Nominee for the Supreme Court could end protections for pre-existing conditions for most New Jerseyans
Because of the ACA, there are 3.8 million New Jerseyans with pre-existing conditions who cannot be charged more if they lose their employer-based coverage and need to purchase insurance in the individual or small group market. However, the Trump administration has argued in a case filed in Texas that because Congress eliminated the individual mandate, the court should allow insurers to charge consumers based on their pre-existing conditions as they did in the past. This would price many consumers out of the market. This threat has become even more serious given that President Trump will appoint a conservative justice to the Supreme Court where this case could ultimately be decided if it is upheld in lower courts. Should the administration get its way on eliminating protections for pre-existing conditions, it could finally unravel the ACA.
New Jersey has taken major actions to protect consumers, but more help will be needed
Thanks to Gov. Murphy and the Legislature, New Jersey was the first state to restore the individual mandate after Republicans in Congress repealed it. This was needed to avoid individuals gaming the system by waiting until they were very ill before purchasing insurance, which would drive up the premiums for everyone else to defray their additional cost. It also discourages individuals from not obtaining insurance and instead going to an emergency room, which would be paid for by taxpayers in the form of charity care payments to hospitals. Most low-income individuals who seek insurance in the marketplace find that their premiums are greatly reduced by federal subsidies and, if they are eligible for Medicaid, there is no cost at all.
New Jersey is also the only state to use the revenues from the individual mandate to help fund a reinsurance program to reduce premiums for middle class families who receive no federal premium subsidies. It has also submitted a waiver to the federal government that would secure $244 million in federal savings starting in the first year and increase thereafter over five years. The combination of these two initiatives would reduce premiums by an impressive 15 percent from what they would be otherwise.
In addition, one of the first acts of Governor Murphy was to sign an executive order requiring all state entities that interact with the public “to provide information to the public regarding the Affordable Care Act and ways to enroll,” subject to budgetary constraints and law. Such a plan to achieve this objective is being prepared by the governor’s office.
These laudatory pursuits will significantly reduce the impact of Republican efforts to undermine the marketplace, but they will not totally eliminate all the harm that will occur. This sabotage would still result in an increase in premiums from what they would otherwise be and possibly more uninsured people. The most effective strategy is for the state and New Jersey’s Congressional delegation to continue to strongly oppose these federal efforts to disrupt the marketplace. However, if that opposition is not successful, the state will need to come up with even more new and creative ways to protect New Jerseyans.