Editor’s note: This report was updated on March 15, 2023 to include new hospital data from RAND and clarify that the cost of hospitals overcharging was $1.2 billion from 2016 to 2018.
Everyone in New Jersey deserves access to affordable health care, yet rising health care prices put high-quality coverage out of reach for far too many. The cost of medical care has outpaced both income growth and inflation for decades, driven in part by increasing hospital prices.[1] When hospitals charge beyond what’s needed to cover their daily operating costs, working families pay more for the same level of care. Recent spikes in premiums for New Jersey state employees highlight how rising health care costs are also passed on to public employees and state and local governments, stretching their budgets thin and costing the state more than $1.2 billion between 2016 and 2018.[2] By reining in high hospital prices, state lawmakers can make health care more affordable for patients, public employees, and state and local governments alike.
Excessive Prices Cost State and Local Governments Billions
Escalating prices for health insurance coverage are often attributed to increased utilization, costs to cover services, and inflation; however, these changes do not fully account for the significant climbs. This leaves rising prices and profits as not-so-hidden factors that could be costing state and local governments hundreds of millions of dollars each year.[3]
In New Jersey, increases in spending have outpaced utilization increases for years.[4] The state health benefits programs for public employees — the State Health Benefits Program (SHBP) and the School Employees’ Health Benefit Program (SEHBP) — are estimated to cover nearly 54,000 fewer people in Fiscal Year 2023 than in Fiscal Year 2015.[5] At the same time, medical benefit costs have increased by approximately $417 million (2022 Dollars).[6] Because of rising health care costs, the state must dedicate more funds toward this coverage each year despite having fewer people covered.
Hospital prices make up a significant portion of rising insurance costs, as the more that hospitals charge, the higher the price of coverage. There is little standardization of hospital prices paid by insurance plans, which are privately negotiated between insurance companies and hospitals.[7] As a result, the “Allowed Amount,” as these prices are known on insurance claims, often exceeds what experts estimate is needed for efficient, quality care.[8] In New Jersey, hospital prices far outpace Medicare rates, which the Centers for Medicare and Medicaid Services sets at amounts that “reasonably efficient providers would incur in furnishing high-quality care.”[9] They also outpace the higher commercial breakeven rate, an estimated “rate a hospital needs to receive from commercial payers to cover all of its expenses for hospital inpatient and outpatient services, without profit.”[10] This includes coverage for uncompensated care, bad debt, and expenses that Medicaid and Medicare do not cover. In New Jersey, the breakeven rate for hospitals is estimated to be approximately 150 percent of Medicare rates.
Claims data shows just how significantly the Allowed Amount for hospital prices in the state health benefits plans outweigh the costs for those same services and procedures at Medicare and commercial breakeven rates. From 2016 to 2018, state health benefits programs paid, on average, prices equal to 230 percent of Medicare rates for inpatient and outpatient care, and 1.5 times the commercial breakeven rate.[11]
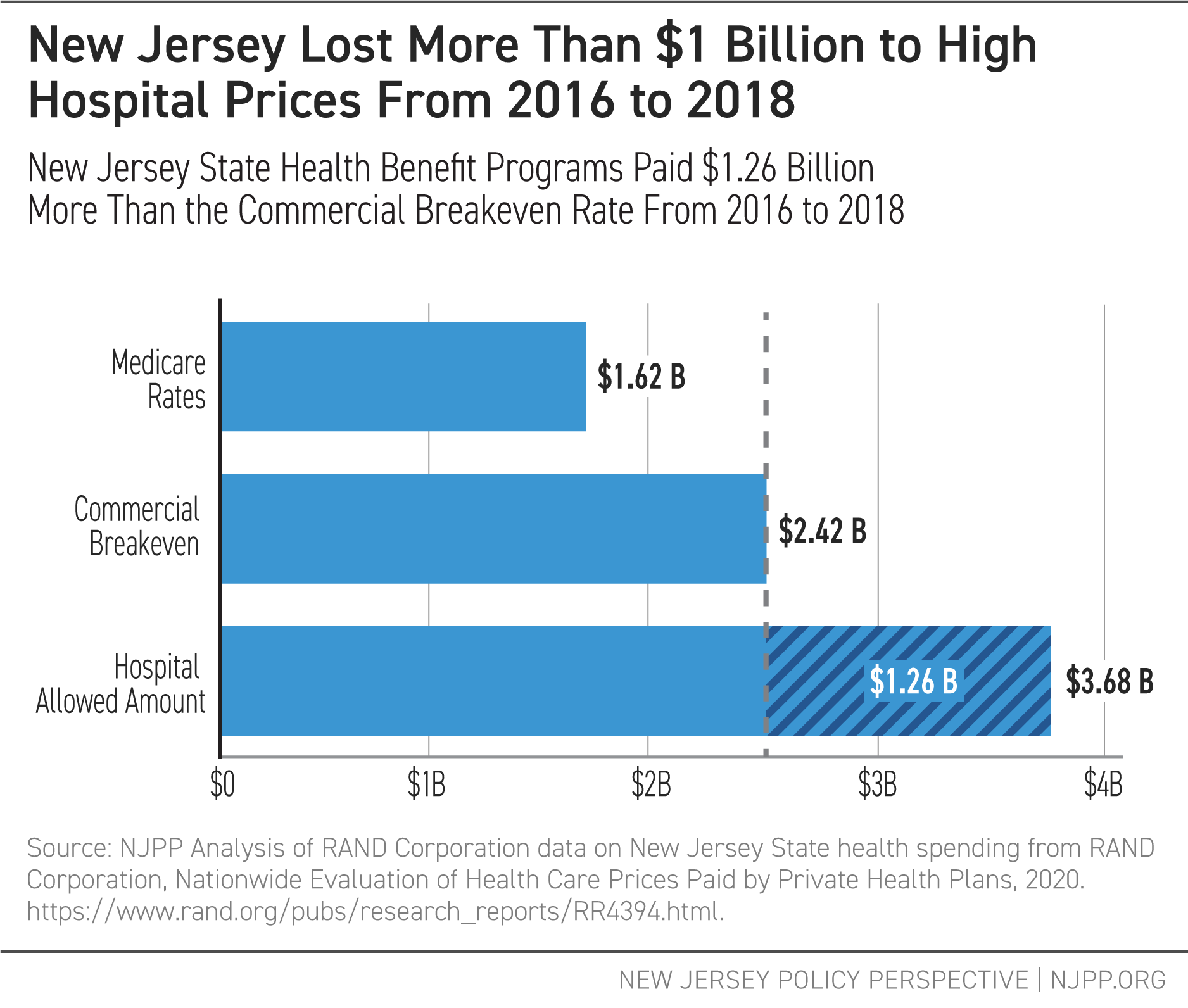
With prices like these, programs like the SHBP and the SEHBP could be paying at least $400 million more per year than what we would expect to cover medical costs if prices were set to cover costs at the commercial breakeven level.
State Lawmakers Need to Rein in Rising Health Care Costs
With the potential loss of at least $400 million every year, New Jersey policymakers should look to better regulate and reduce high hospital prices. Cracking down on rising prices would provide savings to public employees and state and local governments alike, protecting the health care of the public workforce, reducing health care costs, and freeing up funds for other public investments.
While the state’s Office of Health Care Affordability and Transparency has spearheaded a new benchmark program to rein in the growth of health care costs with data-driven analysis, state lawmakers should explore other ways to contain costs driven by hospital pricing, such as price caps and reference-based pricing.[12] To put New Jersey on a path toward a more equitable future, the state cannot simply stick to one-time fixes as bandaids and continue to raise the cost of premiums on public employees and state and local governments. Instead, leaders must do more to rein in hospital costs to control premium costs.
End Notes
[1] New Jersey Office of Health Care Affordability and Transparency, New Jersey Health Care Affordability, Responsibility, and Transparency (HART) Program Blueprint, 2022, pg. 6. http://www.cshp.rutgers.edu/Downloads/Benchmark_Blueprint_March_31_2022.pdf
[2] New Jersey Monitor, Double-digit hike in insurance premiums approved for government workers, 2022. https://newjerseymonitor.com/2022/09/14/double-digit-hike-in-insurance-premiums-approved-for-government-workers/
[3] Health Affairs, It’s Still The Prices, Stupid: Why The US Spends So Much On Health Care, And A Tribute To Uwe Reinhardt, 2019. https://www.healthaffairs.org/doi/10.1377/hlthaff.2018.05144
[4] Health Care Cost Institute, 2018 Health Care Cost and Utilization Report: State Spending Trends, 2019. https://healthcostinstitute.org/interactive/2018-health-care-cost-and-utilization-report
[5] NJPP Analysis of FY 2017 – FY 2023 Budget Detail. New Jersey Office of Management and Budget, Budget Detail FY 2017 – FY 2023. https://www.nj.gov/treasury/omb/
[6] Ibid.
[7] For a study of the variability of prices charged by hospitals, see RAND Corporation, Prices Paid to Hospitals by Private Health Plans, 2022. https://www.rand.org/pubs/research_reports/RRA1144-1.html
[8] HealthCare.Gov, Allowed Amount, 2022. https://www.healthcare.gov/glossary/allowed-amount/
[9] RAND Corporation, Nationwide Evaluation of Health Care Prices Paid by Private Health Plans, 2020. https://www.rand.org/pubs/research_reports/RR4394.html; Centers for Medicare and Medicaid Services, Medicare Inpatient Prospective Payment System (IPPS) & New Technology Add-on Payment Provision, 2020, pg. 2. https://www.hhs.gov/sites/default/files/1.3-treitel-cms-508.pdf; Medicare Payment Advisory Commission, March 2022 Report to the Congress: Medicare Payment Policy, 2022. https://www.medpac.gov/wp-content/uploads/2022/03/Mar22_MedPAC_ReportToCongress_v3_SEC.pdf
[10] The commercial breakeven rate is calculated from annual hospital filings with the Centers for Medicare and Medicaid Services, and takes into account a variety of factors, including patient hospital costs, shortfalls or profit from public coverage programs, administrative costs, revenue from all sources, and much more. The details on how this is calculated can be found at: National Academy for State Health Policy, Understanding NASHP’s Hospital Cost Tool: Commercial Breakeven, 2022. https://www.nashp.org/policy/health-system-costs/understanding-hospital-costs/commercial-breakeven/
[11] RAND Corporation, Nationwide Evaluation of Health Care Prices Paid by Private Health Plans, 2020. https://www.rand.org/pubs/research_reports/RR4394.html; National Academy for State Health Policy, Hospital Cost Tool, 2022. https://d3g6lgu1zfs2l4.cloudfront.net/
[12] New Jersey Office of Health Care Affordability and Transparency, Home Page, 2022. https://nj.gov/governor/admin/affordablehealthcare/index.shtml; New Jersey Office of Health Care Affordability and Transparency, New Jersey Health Care Affordability, Responsibility, and Transparency (HART) Program Blueprint, 2022. https://nj.gov/governor/news/news/562022/docs/20220331a_Benchmark-Blueprint.pdf; National Academy for State Health Policy, Disrupting Hospital Price Increases: Using Growth Caps in Insurance Rate Review, 2021. https://www.nashp.org/disrupting-hospital-price-increases-using-growth-caps-in-insurance-rate-review/; National Academy for State Health Policy, Overview of States’ Hospital Reference-Based Pricing to Medicare Initiatives, 2021. https://www.nashp.org/overview-of-states-hospital-reference-based-pricing-to-medicare-initiatives/

